The Four Stages of Healing

Hi, Dr. Meredith Warner here –
As an orthopedic surgeon, I not only specialize in surgical procedures – but also have to be an expert in the process of healing. Surgery is simply a means to the end – and the goal of each procedure is healing and the promotion of better form and function. I’d like to share a little bit of what I know about the physical process of healing with you today:
There are four main phases of healing that are universal and generally follow the same pattern and timing no matter what. If there is variation, that is when there are problems. Diabetics, for example, have differences in timing between the four phases of healing, which makes their wounds heal slower or become chronic. Each phase needs to function flawlessly and this also can be a source of problems.
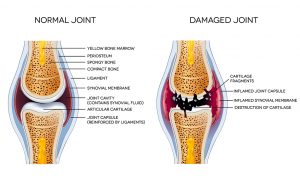
Connective tissue is the stuff that puts a human together and makes the body “stick” together – not just tendons and ligaments. Connective tissue can be bone, ligament, nerves, muscles, tendons and the matrix (surrounding gel/fluid) that holds the cells in place. Its universality throughout the structures of the body serves as a reminder for the interconnectedness of the healing cycle.
The basic building material for connective tissues is often collagen; this is a sort-of woven protein structure. When connective tissue is injured, the collagen must be reformed and the structure of the material (skin, tendon, ligament, etc.) must be re-formed. The human body uses a four-step process that reliably achieves these goals if the environment is right.
The four phases of healing are hemostasis, inflammation, proliferation and remodeling.
Stage One: Hemostasis
Just after an injury, the body is in a default mode to protect and survive. If, for example, an injury results in bleeding, the body stops the bleeding in an effort to preserve the tissue and save energy for possible fight or flight. The body does this primarily through the process of clotting. A clot is a clump of platelets and inflammatory cells that are the first to arrive at the site of injury. They are called to the area by a complicated system of signals released into the bloodstream as soon as an injury occurs.
At the scene of the wound, be it a cut, laceration, contusion, burn, chemical exposure, tear or anything, the platelets bind the exposed collagen of that tissue within the extracellular matrix. Once bound, the platelets begin to work.
Platelets are magical fragments of cells in the blood stream with awesome healing capacity. These begin to immediately secrete sphingosine-1-phosphate, thrombospondin, fibronectin, von Willebrand factor. These then stimulate even more platelet action, promoting a release of clotting factors, which stop the bleeding – by causing a matrix of fibrin to develop that acts as a plug. This stable clot/plug then acts as a bed for substances and cells flowing into the wound, because the platelets in a clot also secrete growth factors that are integral to the next steps in healing.
Platelets release the following substances; many of these have been looked at by pharmaceutical companies separately as potential profit centers:
- Transforming growth factor Alpha – TGF-alpha
- Transforming growth factor Beta – TGF-beta
- Insulin growth factor – IGF
- Platelet derived growth factor – PDGF
- Interleukin-1- IL-1
Once these are released by platelets into the wound environment, other cells like neutrophils and macrophages enter the zone. PDGF recruits cells that form fibrin (fibroblasts) and then collagen begins to be deposited – beginning the tissue repair process.
Stage Two: Inflammation
The hemostasis phase starts immediately after an injury and overlaps with the inflammatory phase of healing. The inflammatory phase should only last a few days. If it persists, then chronic inflammation results and then chronic non-healing or poorly healing tissue is the outcome. For now, we will focus on a normal inflammatory phase of healing.

There is a group of signalling molecules in the bloodstream known as the ‘complement’ system. The complement system is activated at the time of the inflammatory phase. The system brings mediators that control the ‘leakiness’ of the surrounding blood vessels and also signals to neutrophils (inflammatory cells) to enter the zone; complements are chemotactic factors. These chemotactic molecules also attract other white blood cells (leukocytes) within 24-48 hours after the injury.
Mast cells (a type of leukocyte) appear as well and release granules filled with histamine. This is what causes what we think of clinically as inflammation. Mast cells and histamines are directly responsible for the redness, warmth, heat and pain of inflammation. Basically, the “leakiness” of the blood vessels in the region is increased by histamines and that allows for more healing and building cells to reach the zone of injury. This is distinct from the earlier hemostasis phase during which other chemotactic factors induce constriction and ‘tightness’ of vessels to help stop bleeding and allow for clots to form.
One of these cells of inflammation is the neutrophil. Neutrophils remove bad things from the wound; they act to remove pathogens, damaged matrix, dead cells and foreign material. Neutrophils do this by phagocytosis; this is literally the ‘eating’ of the bad stuff. These are early and aggressive cells that begin the process of healing. One can think of this aspect of wound healing like one thinks of the demolition phase of construction.
Next, monocytes and lymphocytes enter. These become macrophages. Macrophages are the workhorses of the demolition process. These cells remove remaining dead and damaged tissues. The macrophages are more selective and powerful than the neutrophils and they do a more ordered and detailed “clean-up” of the damaged tissues. Macrophages remove neutrophils in a very orderly process that prevents damage to normal tissues in the area.
Macrophages are also important because these cells also produce more healing factors. They make more TGF-beta, PDGF, Tumor necrosis factor-alpha (TNF-a) and also cytokines like Il-6, Il-1. All of these growth factors and cytokines from macrophages act to cause the fibroblasts (fiber forming cells) to grow along with smooth muscle and endothelial cells. Endothelial cells are lining cells for vessels and skin.
Once the macrophages have finished cleaning up the injury site and started the healing and rebuilding process by providing the building blocks, they then remove the neutrophils – the cells that clean up debris and were one of the first cells that reach the injury. This is one way that scientists can mark the conversion from the inflammatory phase to the proliferative phase; they can count the neutrophils.
Stage Three: Proliferation
The proliferation phase is the actual construction phase of the tissue. Here is where the connective tissue is made whole again.
The fibrin and fibrin matrix that was produced at the inflammatory phase is merely a scaffold for the actual tissue. It is ‘granulation’ tissue and must be converted to the actual tissue needed; this may be smooth skin, strong tendons and ligaments, muscle or bone. The fibrin is replaced by collagen. This process usually starts on day 2 or 3 after the injury or surgery.
Proliferation involves angiogenesis (forming of new blood vessels), tissue granulation, re-epithelialization (formation of skin) and wound contraction (making a wound small). The main structure of the injured tissue is rebuilt. Mesenchymal stem cells promote the formation of the new tissue types.
The formation of new blood vessels is important because without blood nothing can heal. Blood brings oxygen and nutrition. Blood also allows for the efficient removal of waste. Different growth factors are released that signal for this process to happen. These are:
- VEGF-A vascular endothelial growth factor-A
- FGF-2 fibroblast growth factor 2
- PDGF
- TGF-beta
The growth factors that are released also stimulate fibroblasts to make more growth factors that start the process of skin production as an example. Skin building cells, called keratinocytes flow to the injury site through the bloodstream and enter from the edges of the wound. Keratinocytes are essentially stem cells that have been directed to become skin forming cells. Fibroblasts come from bone marrow when they respond to the chemical signals released during the inflammatory phase. These produce a matrix that allows for the specific tissue to build. The matrix is made of proteins like collagen, fibronectin and hyaluronan. The fibroblasts are stimulated to produce by the PDGF and EGF that the macrophages make.
Some fibroblasts will turn into ‘myofibroblasts.’ These have a muscular component and will literally pull the edges of the wound together to make it smaller as it heals.
Stage Four Remodeling
Wound remodeling is the last phase of healing and its success relies heavily on how well the other three phases of healing went. It usually starts at week 2 or 3 and can last for a year in some cases. In this phase the tissue matures and becomes its true self.
Weaker collagen is replaced by stronger collagen. Disorganized tissue becomes organized. The organization process is regulated by the fibroblasts that secrete an enzyme that degrades the collagen matrix of the wound bed and allows for the realignment of that collagen into organized networks. That organization is modified by stress, load, pressure, gravity and other mechanical and chemical forces. The key to good wound repair is the remodeling and re-organization of the extracellular matrix of the damaged tissue.
How We Prepare For Your Healing At Warner Orthopedics & Wellness
Let’s discuss the specific example of a nerve release surgery for pain. After we perform a nerve release surgery for you we respect this human healing cascade and integrate the paradigm into our rehabilitation protocols.
To promote proper healing, we start motion and deep tissue massage at day 3. This allows us to prevent the extracellular matrix of the healing tissue from depositing back onto the nerve and prevents scar from forming on that nerve.
We have designed a protocol that enhances the healing phases in a way to optimize the healing of both the visible scar and also the underlying structures. Early load uses mechanoreceptors to allow the tissues to realign in a meaningful and useful way rather than in a disorganized mess. Motion is important too such that the granulation tissue that begins to form on day 1 can be placed in a natural way that allows for natural movement of the structure under which we released the nerve.
Our protocol uses fascial stretch and release, deep tissue massage, guided early motion, early weight-bearing and dry needling to promote the appropriate healing along good tension lines and in a strong but non-painful way.
We use a variation of this methodology for every operation or treatment – in my experience, functional recovery is often the best method for healing and can be applied to most procedures.
We also recommend a group of vitamins and minerals that are vital to the immune system and the healing cascade as well as the rebuilding of connective tissues. Our Well Theory multivitamin, developed by Dr. Meredith Warner, can be easily incorporated into your day to help you promote wellness and healing from the inside out.
We at Warner Orthopedics & Wellness are dedicated to helping you recover and get back to you life in the fastest and healthiest way possible.
Contact us today to learn more or to schedule an appointment!